Participating in this Q&A article are Bilal Shafi, MD, from Sutter Health in Santa Cruz, California; Wilson Szeto, MD, from Penn Presbyterian Medical Center in Philadelphia, Pennsylvania; and Grayson H. Wheatley III, MD, Wheatley Surgical in Nashville, Tennessee.
Q: What does an aortic dissection case look like at the hospital?
Wheatley: It happens out of the blue. Sudden pain in the chest or back, a tearing sensation, and waning consciousness sends someone rushing to the ER, where a doctor explains that it is “type A aortic dissection,” a condition in which the layers of the aorta tear. A rupture to the aorta could cause massive internal bleeding, so dissection carries a high risk of death. In fact, it’s not uncommon for patients to die before they can get help. The only option is emergency surgery. For surgeons, the situation is both high-pressure and complex because there is so much variability in both the anatomy and the tears. We must work quickly to determine the location of the tears, choose the most appropriate approach and get the patient into the OR.
Q: What does that time pressure look like inside the OR?
Szeto: This is a long operation – generally about four to six hours, which is the limit on how long the heart and the patient will tolerate the procedure and survive. The first objective is fixing the ruptured or dissected aorta. Objective two is keeping the organs of the body perfused during the operation. During the procedure, we must not only stop the heart, but also interrupt circulation during certain portions of the procedure. Thus, we must apply various strategies to perfuse the organs throughout the procedure. Expeditious conduct of surgery is therefore very important, especially for the brain, since damage may occur if perfusion and protection are inadequate, resulting in a stroke.
Shafi: In the OR, we’re trying to repair fragile aortic tissue, like reassembling layers of tissue paper and suturing them together with a graft. Although we need to work fast, we also want to address the problem thoroughly and effectively. For example, when patients have dissection in the aorta and the descending thoracic aorta or the aortic arch, we want to fix all the tears. But time limitations mean we sometimes have to repair the aorta and leave the residual dissection to be fixed in a second surgery later.
Wheatley: Patients have better long-term survival, lower risk of stroke and better outcomes after surgery if we replace the aortic arch during the initial aortic dissection repair. It’s a much more involved and extensive proposition, and the challenge is to do it safely and quickly because it can add up to 30 minutes to that critical period of circulatory arrest. Thankfully, we’ve seen a lot of research and new techniques to help us treat both problems.
Q: Do you think it will become the norm to perform both procedures at once?
Wheatley: Yes. We’re seeing development of hybrid medical device technologies – a combination of standard surgical needle-and-suture technique with suture-free anastomosis devices to provide integrity of the arteries. New medical devices could facilitate a hybrid approach to aortic arch surgery, making the procedure faster, safer and easier to perform. Any time we can decrease the impact and intensity of surgery – even major, complex, six-hour surgery – we also may speed up postoperative recovery and get patients back on their feet.
Q: What new advances are in the pipeline for aortic dissection surgery?
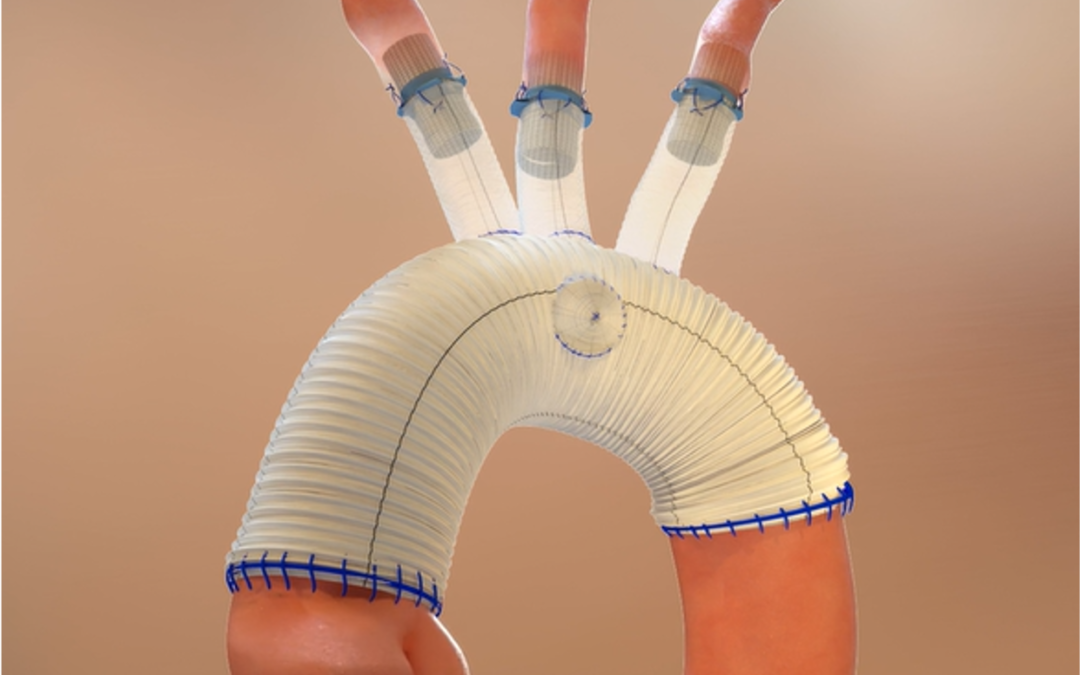
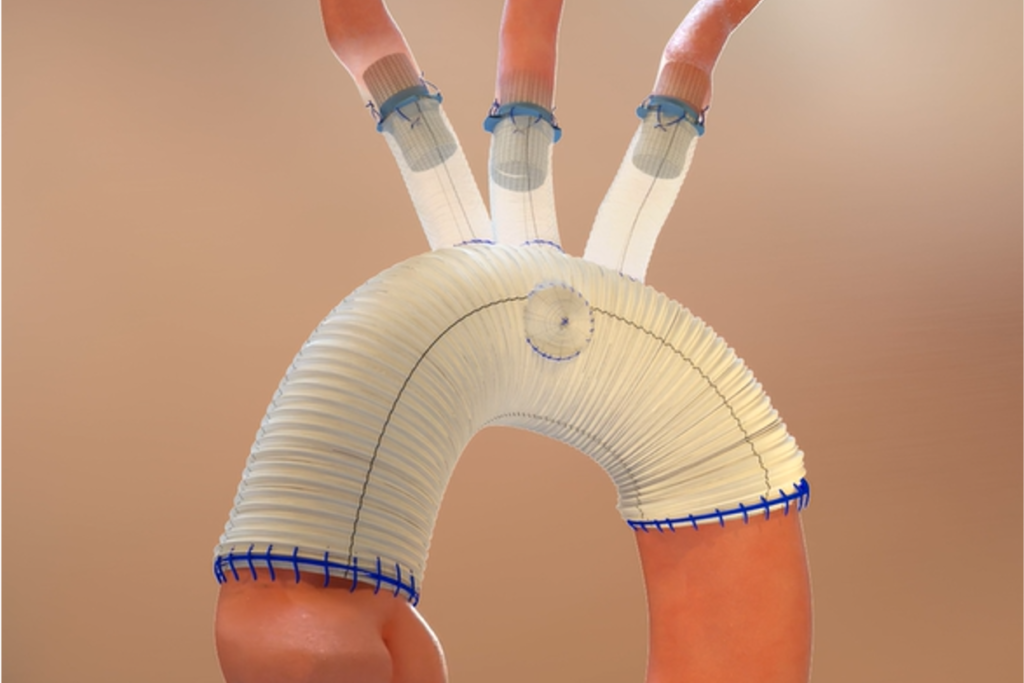
Shafi: We’ve been anticipating a graft for total arch replacement from Terumo Aortic called the Thoraflex Hybrid, which is used in Europe. Its hybrid design, combining woven surgical grafts and stent grafts, could make it much easier to perform total arch replacement. I’ve also been involved with the Aquedeon Medical Duett Vascular Graft System, which is designed to facilitate anastomosis without sutures. Suturing is time consuming; using a delivery system to deploy an anastomosis device that connects a surgical graft to an artery would be much quicker.
Szeto: I agree, this type of graft system has the potential to let us repair aortic dissection just as well as we do now, but easier and faster than we can with hand suturing. Arch vessel connections or reconstruction also could be performed in a technically more reproducible and predictable way, removing some of the human factor of suturing. Any time we can make something more reproducible, we hope the conduct of operation and ultimately the outcomes can have less variation and be improved.
Q: Ultimately, what do you want the new techniques to help you achieve for patients with aortic dissection?
Shafi: We discussed the challenges – the perfusion strategies, the risk of bleeding and the desire to treat everything at once under immense time pressure. I’d add that making the procedure easier to perform could save lives. I’ve seen many patients who were transferred from other hospital ERs because the surgeons there were not comfortable performing this surgery. Unfortunately, some of those transferred patients have ruptured because they didn’t reach us until two hours after their diagnosis. If new techniques can make it easier for the average heart surgeon to perform this surgery, we will get patients into the OR faster and ultimately save more lives.