Studies Show That Zip Reduces Incision-Related Problems and Associated Costs by 50 Percent, and Provides Greater Range of Motion, Less Pain and Superior Scar Quality
ZipLine Medical, Inc. today announced publication of positive results from two significant clinical studies in two peer-reviewed journals demonstrating that use of Zip® Surgical Skin Closure leads to better clinical outcomes and healthcare cost savings than do surgical staples.
A randomized, controlled, prospective study on patients undergoing same-day bilateral knee replacement conducted by Rodney Benner, MD, of the Shelbourne Knee Center in Indianapolis, Indiana, was published in the July online edition of the Journal of Knee Surgery. The study found that the Zip device provided statistically significant clinical and patient satisfaction benefits when compared to surgical staples. Patients demonstrated greater range of motion two weeks post-procedure during recovery and less pain on the knee closed with the Zip device compared to their stapled knee. In addition, patients, the surgeon and a blinded panel of plastic surgeons all preferred the scar quality on the Zip-closed knee.
“The Zip closure improved the patient experience, and as a result, I have changed my practice to include Zip closure in all knee arthroplasties,” said Dr. Benner. “Patients reported less pain, improved cosmetic outcomes, and even improved early function by improving range of motion.”
A separate health economics study of the Zip device conducted by Roger Emerson, MD, of the Texas Center for Joint Replacement, Plano, Texas, was recently published in the online journal Cureus. The study of 130 total knee replacement patients consisted of a retrospective chart review of patients receiving staple skin closure that was compared to a prospective case series of patients receiving the Zip device. Patients receiving staples had more incision-related phone calls to the clinic, incision-related ER admissions, incision-related clinic visits, and antibiotics prescribed due to incisional complications than the patients with Zip closure. The clinic cost for a problem staple patient was almost double that of the Zip group ($27 versus $14.75, respectively), while the opportunity cost for a problem staple patient was quadruple that of the Zip group ($228 versus $50, respectively).
“The results of this study provide insight on how a simple change in the closure methodology can lead to potential downstream cost savings, especially in a bundled payment model,” said Dr. Emerson. “In the study, we noticed that patients were apprehensive about staple removal and concerned when they saw redness around their staples, which in some cases triggered antibiotic prescriptions to avoid possible infection.”
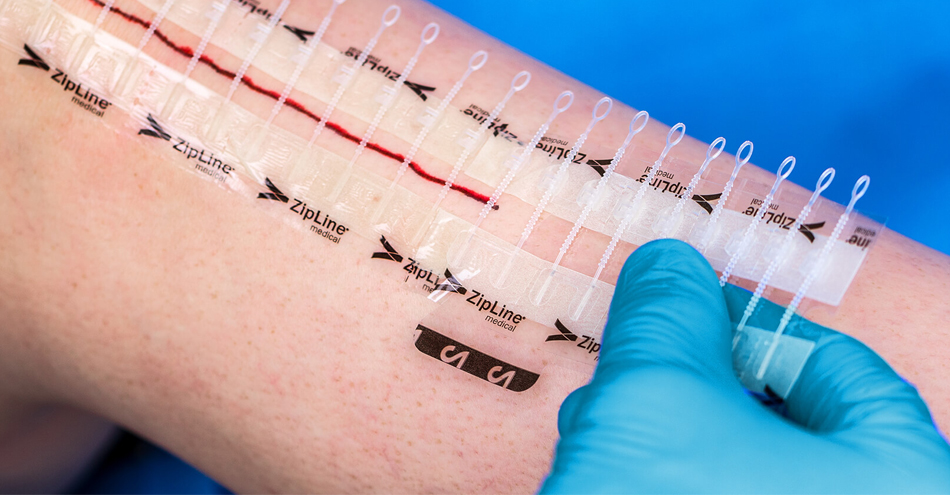
The Zip is a non-invasive and easy-to-use skin closure device that replaces sutures, staples and glue for surgical incisions and lacerations. A patented force distribution design results in secure wound closure, excellent scar quality and high patient satisfaction. Unlike staples or sutures, there are no skin punctures with the Zip that can create pathways for bacteria. Multiple clinical studies have demonstrated significant procedure time savings, fewer wound complications and the ability to reduce healthcare costs. Benefits of the Zip have been demonstrated in clinical studies in orthopedic total joint arthroplasty, spine, foot and ankle, pediatric cardiothoracic, electrophysiology, dermatology, emergency medicine and plastic and reconstructive surgery.