
The United States spends more money on health care as a percentage of gross domestic product (GDP) than any other developed country in the world: nearly 17% of GDP in 2018. This compares to around 10% of GDP in Australia, the UK and Canada.
The average spending for health care as a percentage of GDP among Organization for Economic Cooperation and Development (OECD) nations is about 9%.
And what do we get in return for this spending? Among 11 wealthy nations included in a recent study conducted by The Commonwealth Fund, the U.S. ranked last in health care quality, access, efficiency and equity, as well as indicators of healthy lives such as infant mortality.
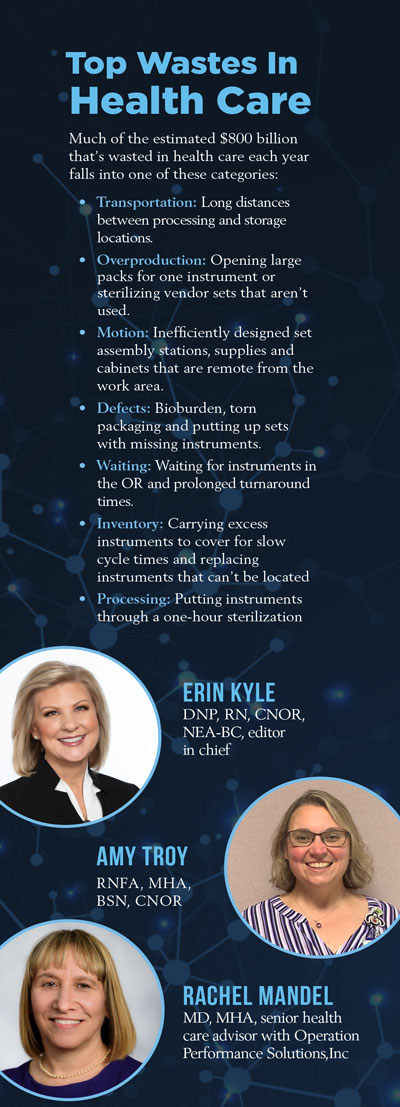
“The U.S. health care industry has been struggling with process improvement, quality and cost for a long time,” says Rachel I. Mandel, MD, MHA, senior health care advisor with Operation Performance Solutions,Inc. (OPS). “The amount of waste in health care is estimated to be 25% of the total spend, or more than $800 billion a year.”
Statistics like these make now the time for adoption of Lean Six Sigma (or Lean for short) methodologies and tools in health care, and in the perioperative area in particular.
“Because Lean principles and tools are intended to help teams work together to identify waste and improve processes to decrease waste, these principles are perfectly suited for application in the perioperative setting,” says Erin Kyle, DNP, RN, CNOR, NEA-BC, editor in chief, Guidelines for Perioperative Practice.
Powerful Operational Philosophies
 Lean principles originated in the automobile industry where they were originally derived from the Toyota Production System, says David Taylor, MSN, RN, CNOR, the president of Resolute Advisory Group LLC.
Lean principles originated in the automobile industry where they were originally derived from the Toyota Production System, says David Taylor, MSN, RN, CNOR, the president of Resolute Advisory Group LLC.
“These principles are powerful operational philosophies that can help health care organizations, including surgical services, improve their performance,” he says.
Although Lean is generally associated with manufacturing and the automobile industry specifically, its philosophies and methodologies can be applied to the operating room, says Mandel. “Process improvement is focused on achieving better results by removing waste,” she says.
Taylor stresses that non-health care organizations have utilized Lean methodologies for several decades to eliminate waste, decrease expenses and improve efficiency.
“This approach to problem-solving can be successfully applied to health care process improvement projects,” says Taylor. “Research has shown that the elimination of wasted steps and the ability to perform certain tasks in parallel to others can significantly improve efficiency in the operating room.”
Mandel lists a few other factors that make this an especially good time for health care organizations to adopt Lean, including the COVID-19 pandemic. “COVID has exposed the gaps in care, especially for the underserved and underinsured,” she says. “Some of these processes were broken even before COVID.”
There’s also the need for hospitals and ambulatory surgery centers (ASCs) to become more nimble. “We have a big opportunity right now for improvement,” says Mandel.
Reduced waste and cost savings aren’t the only potential benefits of Lean in the health care setting. Robert Klym, chief operating officer with OPS, places improved patient outcomes and experiences at the top of his list of benefits.
“Guaranteeing ‘Quality at the Source’ is a core tenet of Lean systems,” says Klym. “We always want to have things done correctly the first time. This intense focus on quality outcomes directly correlates to patient safety.”
Focus on Eliminating Waste
Klym defines Lean as “a set of principles, systems and tools that strives to develop a strong organizational culture. The objective of Lean is continuous improvement through relentless focus on the elimination of waste by every person, at every level, on every process, every day.”
Kyle lists a number of different lean tools that can be used effectively in the health care setting:
- 5S (Sort/Set in order/Shine/Standardize/Sustain) – This can be used to organize and maintain storage areas for positioning equipment and supplies.
- Gemba (the real place) – Here, perioperative leaders make it a priority to systematically spend time where the work happens, such as in the OR, PACU and sterile processing departments.
- Just-In-Time (JIT) – JIT inventory planning has been effective in reducing the amount of inventory on hand and costs associated with storing this inventory, as well as improving control of product expiration while on the shelf.
- Value Stream Mapping – This powerful tool allows visual mapping of processes in the perioperative environment.
In fact, the foundation of a strong Lean organization is built on the stability and standardization of its processes, says Klym. “One example is standardizing instrument packs in an OR so surgeons are confident they will have the tools they need at the time of surgery,” he says.
Creating process and equipment stability within the sterile processing department is another example. “This helps ensure that surgeries are not delayed because of equipment breaking down or not running at a consistent rate, thus causing delays or the need to purchase excess instruments,” says Klym.
A Lean Success Story
Amy Troy, RNFA, MHA, BSN, CNOR, says that Randolph Health, a small rural hospital in Asheboro, North Carolina, where she previously worked, realized numerous benefits by implementing Lean concepts. “The Huddle was the single most effective Lean tool for us,” she says.
As the name suggests, the Huddle involves getting together and talking through issues and problems as a group. “The Huddle created more open communication not only in the OR but also within the anesthesia, sterile processing, PACU, SDS and other departments,” says Troy.
Creating Kaizen boards with OR statistics was another effective Lean application at Randolph Health. “Some of the items tracked on the boards included on-time starts, turnover time, OR utilization and supply discrepancies to ensure we were capturing charges,” says Troy. “No one, including surgeons, wanted to see their name in last place on the board.”
By implementing a Lean concept known as Kanban, Randolph Health was able to cut its annual cost of supplies in half – from $1.3 million to $635,000. “This affected multiple departments including materials management, which had to be on board with the program,” says Troy. “And it was a hard sell for the OR staff, which wanted 100 items in the supply room bins.”
Process mapping was yet another effective Lean tool Troy used at Randolph Health. “This helps you look at the inner workings of a process and it really makes the gaps pronounced,” says Troy.
“Having staff sit down and talk about the way they work is an eye-opening experience,” Troy adds. “Nothing works better than a process map to point out gaps that need attention so staff can function more efficiently.”
Troy summarizes some of the potential benefits of adopting Lean practices in the OR:
- Cost savings, including lower inventory levels and less staff overtime.
- Greater staff satisfaction due to more flexible scheduling.
- Higher patient satisfaction scores due to shorter wait times and a more streamlined patient flow.
- Happier surgeons due to better patient outcomes.
- More repeat business from satisfied patients who return for future surgeries.
Lean Challenges and Keys to Success
The single biggest challenge to implementing Lean in hospitals and other health care organizations, says Kyle, is the magnitude of change in mindset and operations it requires.
“Getting every leader and each of their teams to embrace the change is no easy task,” says Kyle. “Ultimately, the success of Lean is dependent on organization-wide adoption.”
Troy believes that the biggest key to a successful Lean implementation is getting OR staff involved early.
“There’s often a fear of losing jobs because staff hear that Lean is all about reducing manpower,” she says. “So managers need to explain to staff that Lean isn’t about losing manpower – it’s about maximizing the productivity of the existing OR staff and helping prevent burnout.” Mandel agrees.
“The OR staff needs to be a part of the solution and contribute to the process so they understand the rationale behind the changes,” she says. “Otherwise, they won’t embrace it or commit to it.
“Ultimately, the goal of Lean is to create culture change,” Mandel adds. “Lean is not a ‘project’ – it’s a way of thinking.”
Klym stresses the importance of getting Lean buy-in at the top of the organization.
“Very few Lean initiatives are successful without executive sponsorship,” he says. “Lean success starts at the executive level with things like strategy alignment and continues with executive engagement as active members of the implementation efforts.”
Health care organizations should focus more on the cultural aspects of Lean, Klym adds, and less on the technical and engineering principles and language. “The use of Lean technical terms can be overwhelming to new adopters, especially those in a health care setting,” he says.
“The real power of Lean is in engaging as much of your workforce as possible in the pursuit of activities that eliminate errors, employee frustration and waste,” says Klym. “You want to empower all employees to become the CEOs of their ‘mini-companies.’ ”
According to Troy, creating a culture that allows staff to feel comfortable with each other and think outside the box is another important key to Lean success.
“Let your staff have full control of the changes brought about by Lean and support them by helping them through the inevitable roadblocks that emerge,” she says.
Taylor recommends that health care organizations hire a consulting firm that specializes in Lean to assess their needs and help with Lean implementation throughout the surgical and procedural areas.
“A consultant who not only understands Lean, but also all aspects of the surgical environment, will give you better, longer-lasting results,” he says.
Some Lean Best Practices
Mandel suggests that perioperative nurses discuss their interest in Lean ahead of time with leadership in order to get buy-in and initial resources.
“Explain your rationale for why you think Lean is important from a patient safety and quality care standpoint,” she says. “Start with something that is a pain point for everyone, including the surgeons, and then pilot an initiative that can be used to support the adoption of a broader Lean strategy.”
Troy emphasizes the importance of working on a manageable number of Lean projects at a time. “Don’t work on multiple Lean projects at once because staff will get overwhelmed with all the changes and shut down,” she says. “Then you’ll loss the support from staff and the changes will not stick.”
Perioperative managers also need to understand that there’s no one-size-fits-all Lean solution for every situation. “Moving toward better outcomes is the key,” says Troy. “Think of lean tools as being a method of continuous improvement.”
According to Klym, one of the biggest complaints patients have about health care is delays and having to wait for their surgeries and other procedures. “With so many patients now having the ability to choose where they receive care, it’s more important than ever to create a positive patient experience,” he says.
“Health care organization can decide to invest in more comfortable chairs and nicer TVs in their waiting rooms, or they can adopt Lean systems that aggressively attack processes that might lengthen patients’ wait times,” he adds. “I believe investing in Lean is a better choice.”









